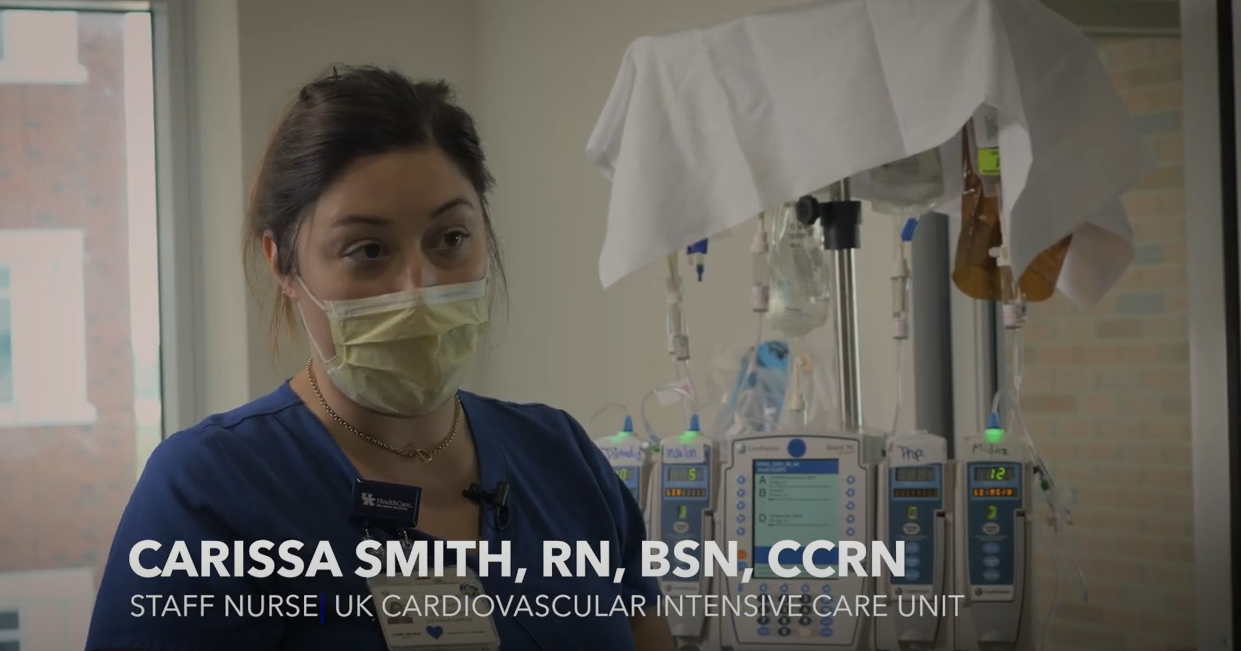
Voices from the Front Lines: Carissa Smith
We recently joined hospital staff for a few days to document the reality of treating COVID-19 patients in UK HealthCare clinical settings.
This edited interview is part of our ongoing series, “UK HealthCare: Voices from the Front Lines,” highlighting stories and perspectives from our frontline staff who have been caring for the sickest COVID-19 patients since March 2020.
Carissa Smith, RN, BSN, CCRN, has been a nurse in UK HealthCare’s cardiovascular intensive care unit (CVICU) for six years.
Prior to COVID, what kind of patients did you typically help?
We had a lot more surgical patients; we saw a lot more cardiology patients, open-heart cases. We saw a lot of transplants – heart, lung and occasionally kidney transplants.
So (when COVID surges), we’re limited a lot on the different variety of patients we treat. We’ve become more familiar with pulmonary care overall and seeing more internal medicine pulmonary patients.
COVID patients with severe lung damage may be placed on extracorporeal membrane oxygenation, known as ECMO – this is essentially a machine that pumps and oxygenates the patient’s blood for them. Why are these patients now seen in the CVICU instead of the medicine intensive care unit (MICU)?
So during the first waves [of COVID], we didn't have nearly as many ECMO patients. They would cohort them still to the 10th floor (in the medicine intensive care units).
The surgeons would cannulate (insert the ECMO cannulas into the neck and groin), and then the nursing staff from the CVICU are the ones who take care of these patients. So we would go up there. And initially working with these patients, I wasn't as familiar with working around the isolation requirements and all of that.
The medicine nurses and techs (in the MICU) were wonderful, helping me learn, and making sure everybody's safe going in and out. So I think from a nursing perspective, it was a great learning experience to be upstairs and a great situation to be in to learn new things from new people.
However, it's nice to kind of be back “home” in the CVICU. I know what these physicians like. I know how they communicate. I know how a lot of them like to treat their patients. And then it's also really nice to just have familiar faces around you, because it can be very stressful mentally and just stressful in general when the patient's doing poorly.
So it's really great to have the support of people that I've known for years, people that were with me to celebrate my birthday a few weeks ago. So it sounds kind of silly, but it does make a big difference.
What kind of situation would lead to a COVID patient needing ECMO?
These patients typically get worse (from COVID-19), sometimes very rapidly. They might test positive at home, be home for a period of days, then come into the emergency room. Or they have to call an ambulance because they're so short of breath, they can't get themselves there.
So they come into the emergency room, try BiPAP (a non-invasive breathing machine with a mask), and then if they don't get better with that, then they move to intubation with a ventilator, then proning.
Then we move to ECMO, and sometimes we have to prone with ECMO, which is very dangerous. it's definitely a last resort. We didn't think we could get more life support than ECMO and a ventilator, but then we were turning patients over. So it's scary for everyone involved. But if it helps them, we'll try it.
Have there been any moments dealing with COVID over the past year and a half that stand out to you?
I can think of experiences that were not pleasant for me, because there's a lot to pick from there. It's very difficult to see someone become rapidly sick and to the point of death. And I'm (outside the room) putting on all this PPE, but I want to be in there with them trying to help.
I've had trying times talking with patients’ loved ones on the phone, discussing with them the chances that the patient going to make it through this, because those can be scary numbers. However, when we finally do get over the hurdle where they can finally come in and visit, or where I can coordinate for them to at least be able to FaceTime into the room through our eICU, I think that is very satisfying.
It can be disheartening. But then seeing people that I've cared for finally be taken off of ECMO feels like a big triumph for them and their family.




