




“Our goal is to empower caregivers.”
A CD player. Lavender-infused lotion. A weighted blanket. A roll of red tape. The last things you’d expect when it comes to Alzheimer’s care. But every item was chosen for a specific purpose: to help care for a person with Alzheimer’s disease and related dementias through their sense of hearing, smell, feel, sight, and more.



That’s how Dr. Elizabeth Rhodus, an assistant professor at the UK Sanders-Brown Center on Aging, Center for Health Equity Transformation, and Department of Behavioral Science approaches her life’s work. She, along with Dr. Allison Gibson of the UK College of Social Work, are leading an NIH-funded study on a new way to help adults with dementia: not through medication, but through simple sensory changes in their home environment.
Sensory stimulation occurs when one or more of the following senses is activated: vision, hearing, touch, smell, taste, pressure, movement and internal feelings. With the help of basic tools and materials, caregivers can stimulate these senses in adults with dementia in ways that can make them feel safer, happier, and more comfortable. That could mean offering a loved one a weighted lap pad to calm and regulate their nervous system, playing a familiar song to soothe anxiety, or placing red tape in important places around the home for increased visual recognition.
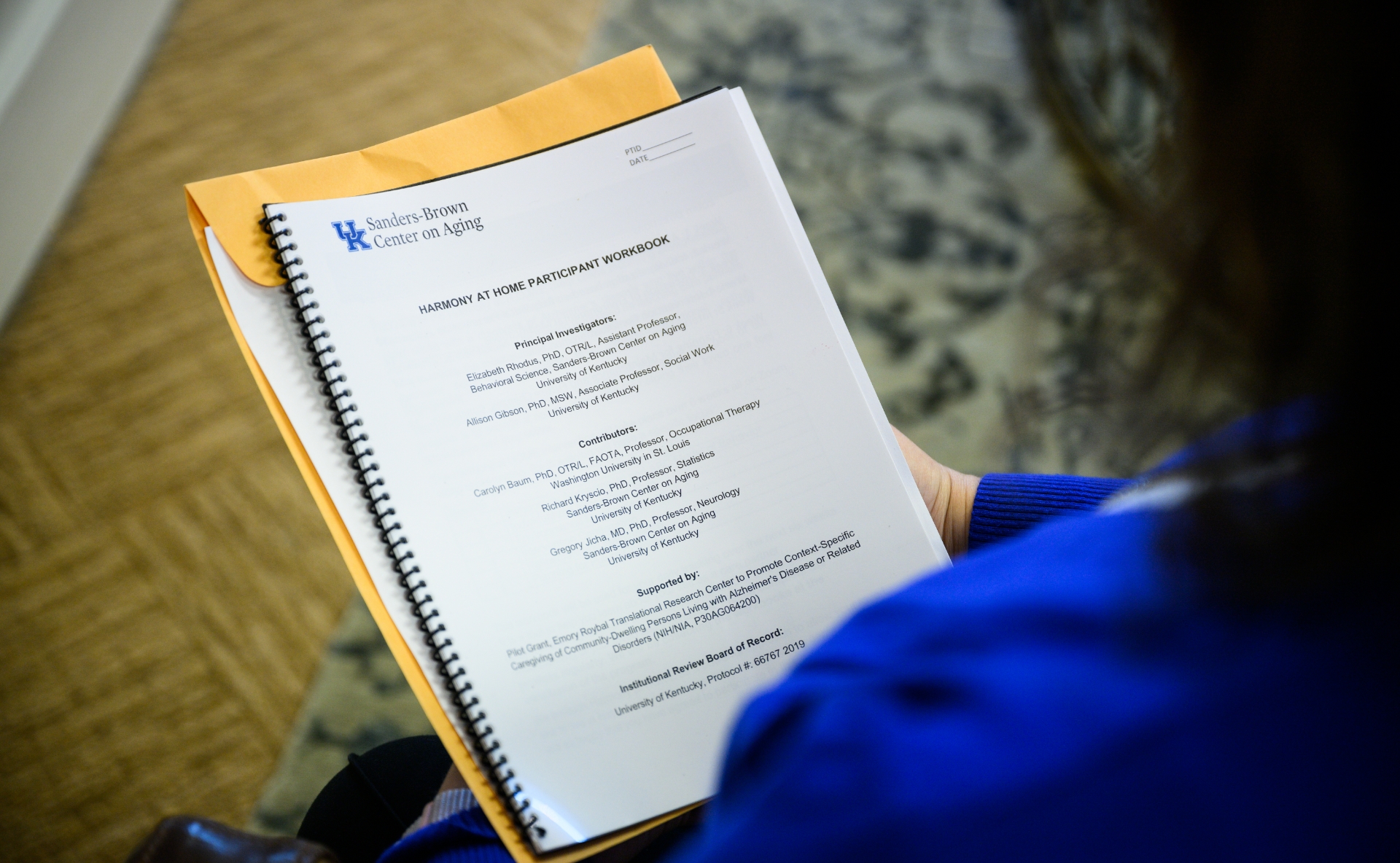
Dr. Rhodus’ study offers caregivers access to the Harmony at H.O.M.E. (Help Online Modifying the Environment) telehealth program, which provides training and tools for care partners to help improve the daily life of the person with dementia. All participants receive a box of practical items that can be used to facilitate sensory stimulation in the home.
“Our goal is to empower caregivers to feel comfortable and competent in recognizing behaviors as a way to communicate,” said Dr. Rhodus. “By providing [caregivers] with training and tools, they can do simple modifiable things in their environment to help support behavior and activity participation for the person for whom they provide care.”








As part of the six-week program, participating caregivers meet virtually with a licensed Occupational Therapist once a week to discuss behaviors, interventions, and modifications for each person with dementia. Caregivers are asked to journal behaviors and keep track of how they’re using the interventions on a daily basis. Telehealth programs like Harmony at H.O.M.E. are particularly relevant for people living in rural communities, where access to health care and caregiver support is not always available.
Laura Henley, a Louisville-based occupational therapist participating in the program, said interventions can be as simple as adding music to a person with dementia’s daily routine, encouraging movement with exercise bands, or changing the lighting in a room. Interventions are personalized for each person—for example, providing water shoes to wear in the shower for someone who is hypersensitive to touch on their feet. Every intervention is a small way to make everyday activities a little easier for caregivers and their loved one.
“I like to let caregivers know there are a lot of different things they can do to help a loved one throughout the day,” said Laura. “But I want them to pick the things they’re going to carry through with, and really implement into their daily routine. We don’t want to add things to be a burden—we want things to be easier.”
“I participated in this program and I highly recommend it,” said one caregiver. “I learned so much specific information that you can’t find online about behavioral and environmental changes that will help someone maintain their independence as long as they can.”
Every caregiving situation is different, and the program is meant to be personalized for the individual needs of each person and caregiver. Designed in conversation with caregivers, the goal is always to make the person with dementia feel safe, happy, and comfortable.
“At every stage and every step, we have to respect the personhood and autonomy of older adults to make their decisions,” said Dr. Rhodus. “But we also integrate where they’re at in the disease process and what they need from a neurological perspective.”
This multi-sensory approach to caregiving is still an emerging idea, but Dr. Rhodus said the NIH is paying increasingly close attention to the relationship between sensory processing and dementia. For instance, NIH studies have found that people with cataracts who have low vision, as well as those with low hearing, have a higher risk of developing dementia. And while there’s still no cure for Alzheimer’s disease, early diagnosis and advances in treatment can offer hope for a better quality of life for those living with this devastating condition.
“There’s been a continual upward trajectory in how we’re caring for people,” said Dr. Rhodus. “We’re seeing longer life expectancies and better outcomes clinically for individuals living with dementia. At Sanders-Brown, we have numerous research projects aimed to develop new medications to treat and cure Alzheimer’s disease. We don’t have a cure yet, but we do have treatments that may slow the progression—and behavioral interventions that can lead to better quality of life.”




