
A Deserving Heart
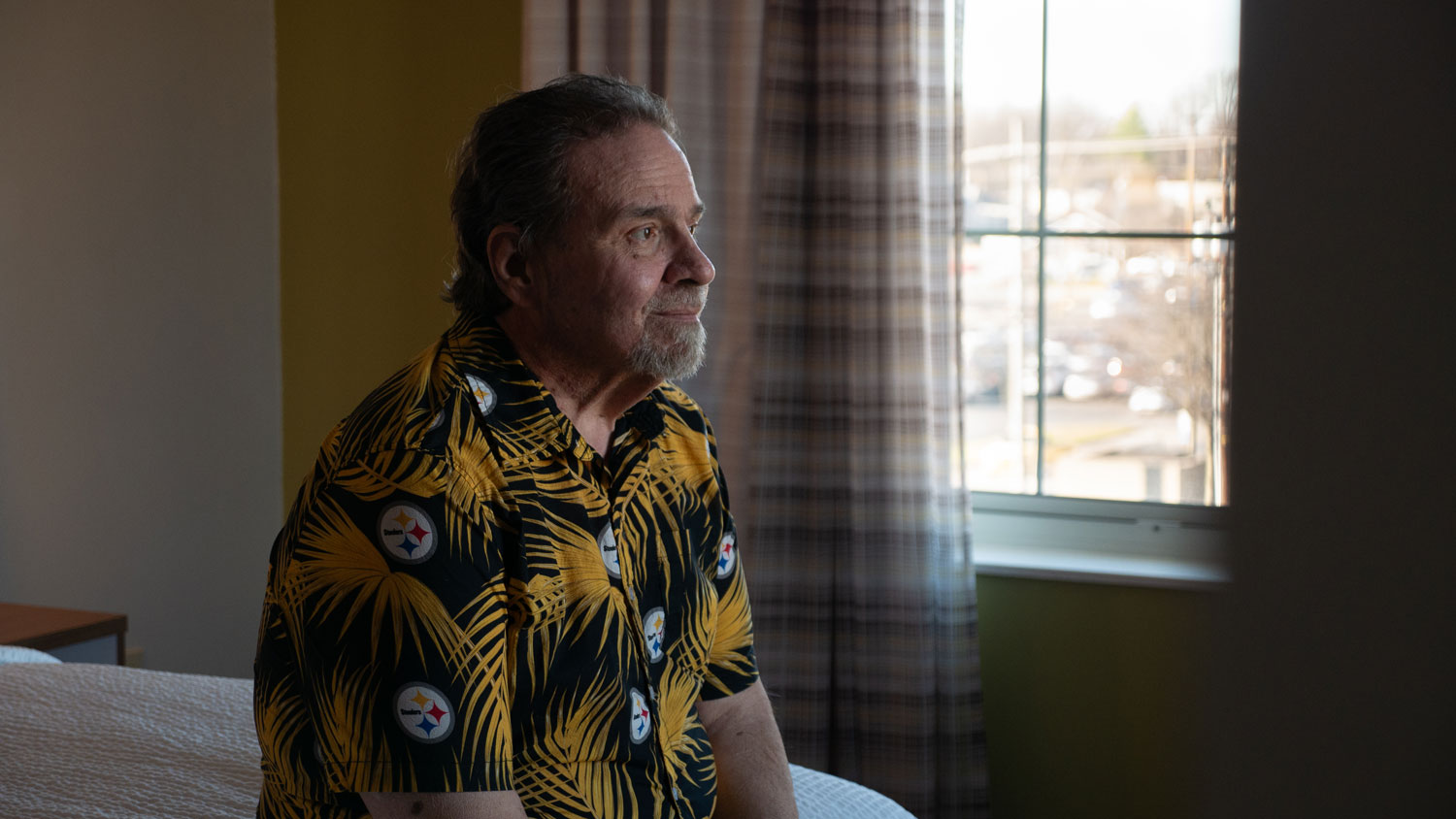
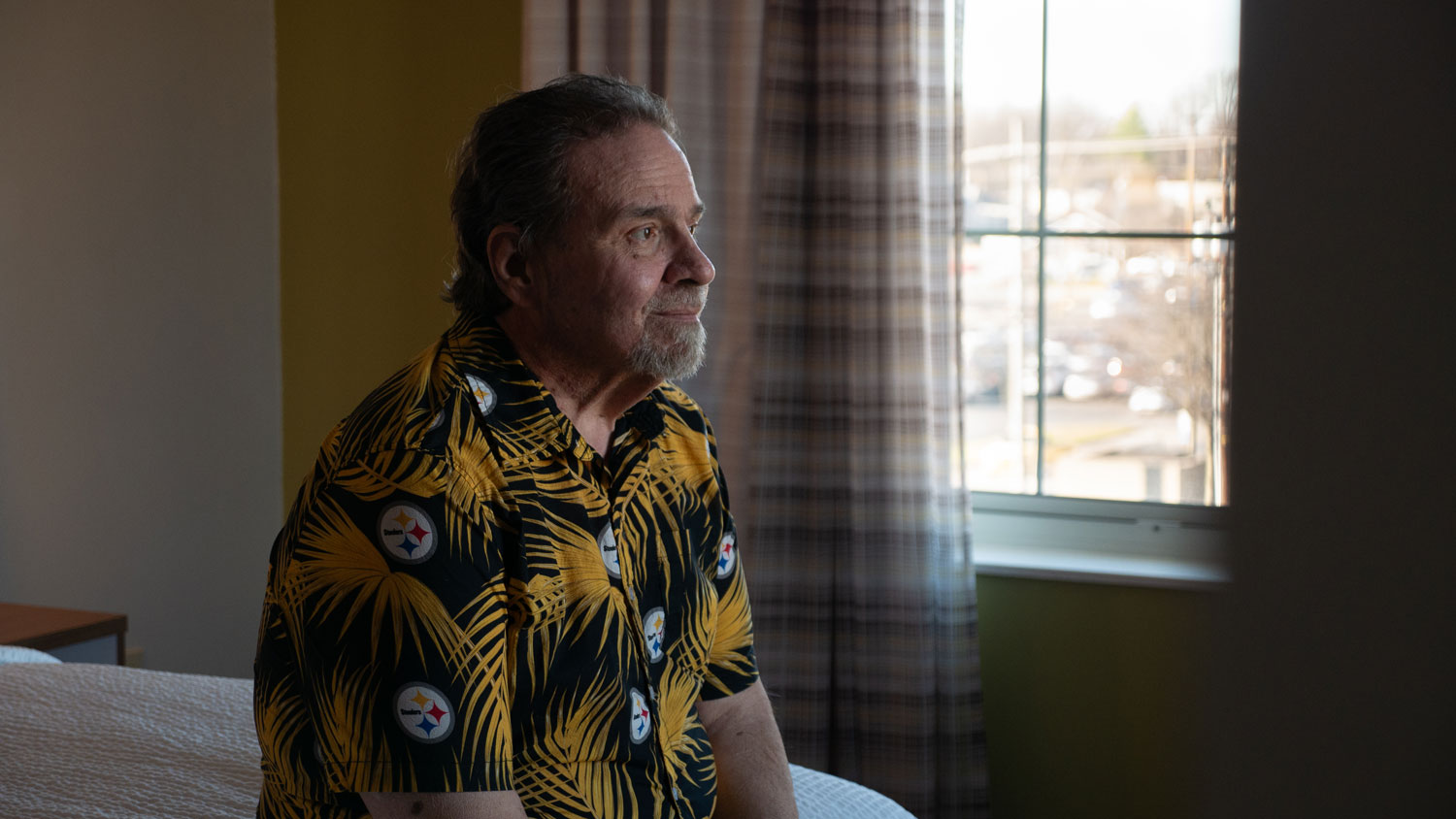
It isn’t exactly clear when Ronald Kelly began experiencing heart failure, because he’s always gone to extraordinary lengths to finish what he starts and put on a brave face during difficult times.
Ronald’s partner, Deborah, thinks his problems first started in early 2012, after they returned home from a cruise. For several days, he just didn’t feel right, but they chalked it up to a bug caught during their trip.
Fast forward to the summer of 2014, when Ronald got home from work — he was a chef in Louisville — and began mowing the lawn. With just a handful of short rows remaining, he stopped and went inside.
“I said, ‘Ron, what's wrong?’” Deborah recalled. “He's like, ‘I'm gonna get this done. But I'm coming in to lay down.’ I think that he had a silent heart attack.”
From that moment, Ronald started seeing a cardiologist in Louisville. His ejection fraction — a measurement of the total amount of blood in your heart that is pumped out with each heartbeat — was reading between 15% and 18% (a normal measurement is from 50-70%). He needed a new heart, even if he didn’t want to admit it.
“He really wouldn’t get into his symptoms or how he felt, and that’s what made it even tougher,” Deborah said. “Ron won’t own it when he doesn’t feel good. He’s that way.”
Fast forward another two years to Ron’s birthday on July 8, 2016. By that point he was part of Deborah’s insurance plan — “His insurance just wouldn’t pay for anything but medication,” she said — and awaiting a heart transplant at an outside institution. However, he was getting worse and Ron was admitted for what would become a three-month stay.
Ron up to that point had refused a left ventricular assist device (LVAD), a surgically implanted, battery-operated pump that helps blood flow. He wanted to continue waiting for a new heart.
“They kept thinking they were gonna get one, and it just wasn’t coming in,” Deborah said. “I finally said, ‘Ron, that’s it. You’re either getting an LVAD or I’m going to get guardianship of you.”
On Oct. 7, 2016, Ron received his LVAD. Unfortunately, Ron’s heart had endured too much: ten days later, he had a massive stroke.
Organ Care System a 'game-changer'
Rehab helped Ron return to a point where he could walk and take care of day-to-day tasks, but he’s since suffered from expressive aphasia — he can understand speech but has difficulty speaking fluently. Deborah now does most of his verbal communication.
The LVAD that he profusely refused did result in a positive impact on his health for about six years, but Ron still wanted a new heart. Unfortunately, the hospital which implanted his LVAD did not think he was a transplant candidate.
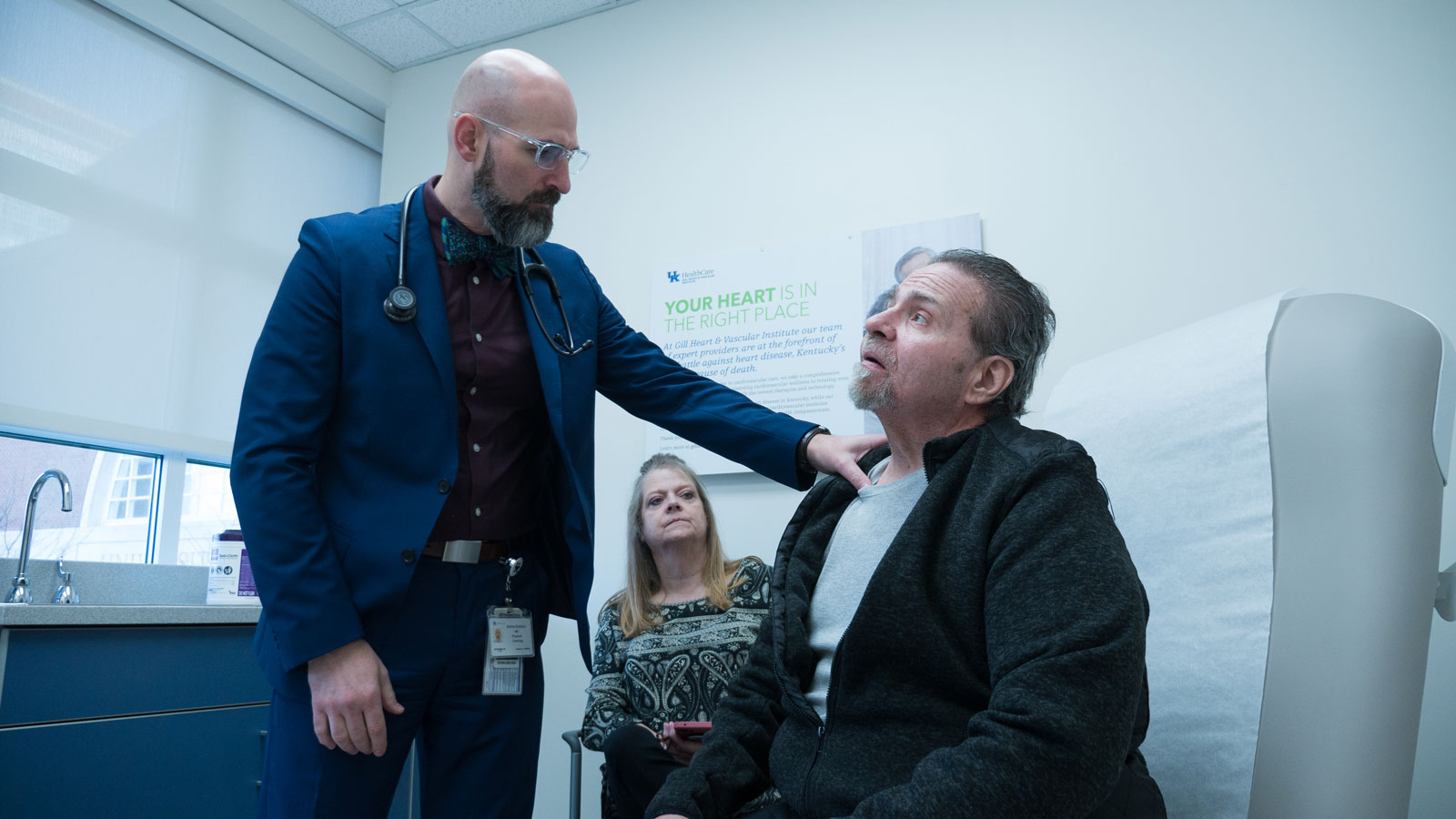
By early 2022, Ron had transferred his LVAD care to Norton Heart & Vascular Institute, where he began seeing a new heart failure cardiologist, Dr. Kelly C. McCants, executive medical director of the Norton Heart & Vascular Institute Advanced Heart Failure & Recovery Program. “When I met Ron it was clear to me he was a man full of life and fighting to have as many years as possible with his family,” said Dr. McCants. “He was looking for hope and after a thorough evaluation, discussing his options with he and his wife, I wanted to connect him to our network of care that would give him every option possible.”
As a member of the UK Gill Heart & Vascular Institute Affiliate Network, Norton Healthcare in Louisville works with UK HealthCare to collaborate on care for patients with advanced heart failure, specifically for patients who may need evaluation for a heart transplant. Dr. McCants referred Ron to UK HealthCare, where he met Dr. Navin Rajagopalan, director of the Gill Heart Affiliate Network. Ron was evaluated for heart transplantation and placed on the transplant list in March 2022; just two months later on May 17, 2022, he was in Lexington for a trailblazing surgery.
Ron was the first heart transplant patient at UK HealthCare to receive a heart transported via the Organ Care System (OCS), a medical device designed by Transmedics that gained first approval from the U.S. Food and Drug Administration in September 2021. OCS devices are designed to keep donor organs in an active state that more closely resembles how they function within the human body.
The device used for Ron’s transplant is colloquially referred to as a “Heart in a Box.”
“Our ability to use the OCS Heart System is a game changer for our patients,” said Dr. Michael Sekela, surgical director of heart transplantation at UK Gill Heart & Vascular Institute. “In the right circumstances, it allows us to use donor hearts our program may not have otherwise been able to accept due to timing or distance. This leads to shorter wait times and better outcomes for our patients.”
Dr. Raj Malyala, the surgeon who led the team that performed Ron’s transplant, said there were “a few bumps in the road,” but overall his surgery couldn’t have gone much better. He was out of the hospital by June 11, 2022, just shy of a monthlong stay. The biggest proof of that is Ron himself, who is the happiest and healthiest he’s felt in a decade. He might still be waiting if not for the OCS transport.
“It doesn’t do any good to have more patients on the transplant list if we don’t expand the number of donors. Otherwise we are just giving people false hope,” Dr. Rajagopalan said. “We are transplanting more patients as a country than we were a couple years ago. It’s not just because of OCS, but the overall result is that we are able to help more people.”
‘You deserve to live if you want it’
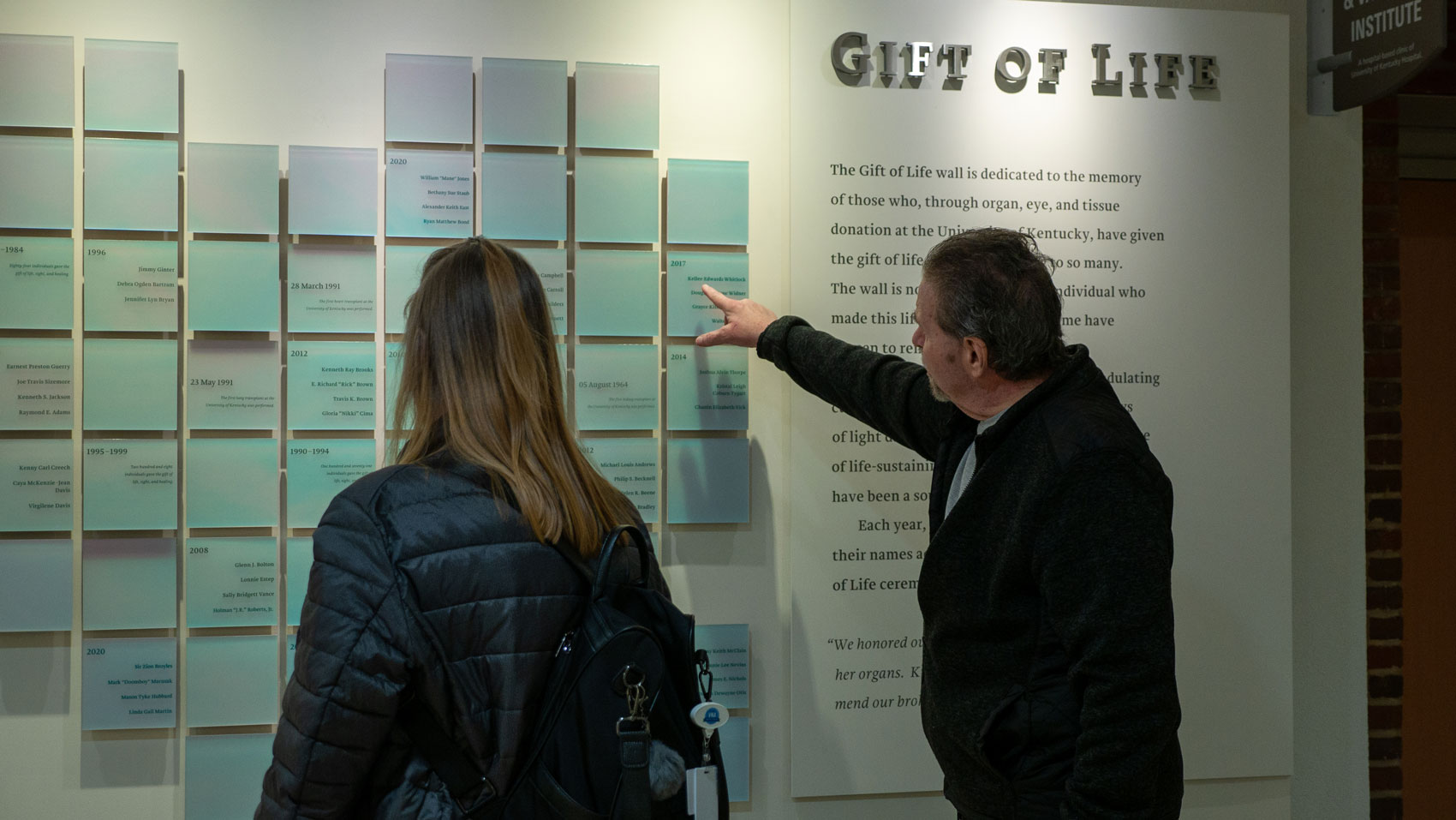
Ron got the heart he wanted, but he and Deborah share concerns about whether to reach out to the donor family and thank them for the gift of life.
Organ donation is a selfless act. When a person who has chosen to become a donor dies, they don’t get to choose where their organs are directed. They could save an 8-year-old girl with years of life in front of her, a billionaire who's gained their fortune through dubious means, or someone like Ron — a man in his early 60’s who’s happy as ever despite the complications he’s experienced since his stroke.
“I’m afraid that if they meet Ron, and he can’t talk, are they going to think that heart was wasted?” Deborah said. “He’s no less of a person because he can’t speak. My fear is they’re going to think, ‘Why wasn’t my heart given to somebody that has young children? Or someone who speaks or who works?”
Though Ron says fewer words these days, the life he is able to live thanks to his heart speaks volumes. He’s back to mowing the lawn, restoring sports cars and spending quality time with Deborah and his two sons. Ron recently celebrated the one-year anniversary of his transplant, and — with things going smoothly — has started to receive follow-up care closer to home at the UK Transplant & Specialty Clinic located at Norton Audubon Hospital in Louisville. He's also received follow-up care from Dr. Andrew Kolodziej, medical director of UK HealthCare's heart transplant program.
To deny Ron a heart transplant solely because he had a guardian would have been unethical, Dr. Rajagopalan says. The evaluation might have been different if he did not have a significant other or guardian to help him communicate, but his neurological condition was never a concern for any of the doctors who cared for him.
“There was a track record of successful care,” Dr. Rajagopalan said. “He had taken care of his LVAD for a long time. If patients are able to take care of their LVAD, it usually means they will be successful in taking care of their new heart.”
Through it all, Ronald’s resolve has remained steadfast and his brave face intact. According to those who know him best, he’s the man he’s always been — just with a healthier heart and an interpreter.
“He wanted it,” Deborah said. “He did everything right. He raised his boys. You deserve to live if you want it. If he wouldn’t have wanted it, I would’ve been like, ‘All right.’ But he wanted it. Every human, every living thing has a right to live.”
And Ron gets to do what he’s always done best: finish what he started.
























